Genicular Artery Embolization
Genicular artery embolization (GAE), or embolization of the knee, is a novel minimally-invasive procedure providing immediate and long term pain relief for patients with osteoarthritis (OA), by reducing the blood flow to the lining of the knee, known as the synovium. It is performed by an Interventional Radiologist (IR), who is a specialist physician that uses X-rays and other imaging modalities to see in the body and treat diseases without surgery.
Osteoarthritis of the knee
- Osteoarthritis (OA) is a leading cause of disability and chronic pain that reduces physical activity and quality of life. OA affects nearly 30 million people in this country, and the knee is the most common site. The prevalence of knee OA has been rising because of the increasing aging population and the obesity epidemic. OA has long been recognized as a “wear and tear” disease; it is now considered a much more complex disease of low-grade inflammation induced by inflammatory mediators released by cartilage, bone, and synovium. Geniculate artery embolization targets this low-grade inflammation.
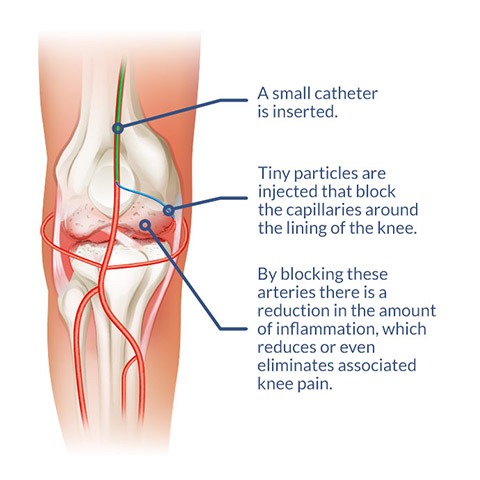
GAE blocks the blood flow to the lining of the knee, known as synovium, that are inflamed. By blocking these arteries, there is a reduction in the amount of inflammation associated with osteoarthritis, a process that can help or eliminate the associated knee pain. While further research is needed, initial trials shows the promise this technique holds for patients with debilitating knee pain who are not ready or willing to undergo knee replacement surgery. While it may not treat the underlying cartilage destruction, evidence so far shows that this may be an effective way to manage the symptoms. In an article published in the Society of Interventional Radiology in March 2021, average pain scores decreased from eight out of ten before GAE to three out of ten within the first week.
GAE is performed with moderate ‘twilight’ sedation as an outpatient procedure, meaning the patient will go home after the procedure. The procedure generally takes one to two hours. Our IR physicians will insert a small catheter (a thin hollow tube) into the artery of the patient’s upper thigh and, with the use of X-rays, guide the catheter to the arteries supplying the lining of the knee. Tiny particles are then injected through the catheter into these arteries, reducing the blood supply. This in turn reduces the inflammation associated with osteoarthritis, which alleviates the pain.

Initial (left) and final (right) angiograms of the knee after embolization. A circular marker was placed at the site of pain. The reduced blood-flow at the site of pain after embolization reduced inflammation of the knees.
Patients go home the same and in most cases, relief begins to occur in two weeks, as the inflammation in the lining of the knee is reduced, relieving the knee pain associated with osteoarthritis.
GAE is a non-surgical treatment alternative for patients with knee pain due to osteoarthritis who have failed conservative therapy, such as anti-inflammatory medications or knee injections, and who do not wish to undergo or are ineligible for knee replacement surgery.
The following conditions make for a good candidate for GAE:
- Age: 40-80 years
- Moderate to severe knee pain
- Osteoarthritis based on x-ray, but without bony deformity/sclerosis
- Local knee tenderness
- Resistant/failed conservative treatment (NSAIDS/PT/joint injection)
The following conditions may disqualify a patient as a candidate for GAE:
- Current or previous history of cigarette smoking
- Advanced arthritis based on x-ray
- Infection or malignancy
- Good candidate for knee replacement surgery
- Is the procedure painful?
– No, we make you comfortable for the procedure with the use medications to make you
sleepy and for pain. After the procedure, you may have some soreness for a few days
for which you may take over the counter medications. - How long does the procedure take?
– The procedure takes about 1 hour. - How long does it take for the procedure to work?
– Most patients feel relief in about 1 week. Some patient experience pain relief almost
immediately. - How long does the pain relief last?
– Most trials show pain relief lasting about 1 year. In some patients, it may last longer. - Can you do both knees?
– Yes, we can do both knees if needed. We do one knee at a time. - What is the recovery from the procedure?
– Recovery is very fast from the procedure. You will go home within two hours of the
procedure. We recommend no heavy lifting or strenuous activity for 3-5 days.
Otherwise, you are back to your normal activity level. - Is it safe to close an Artery going to my knee? Don’t I need the blood circulation to that area?
– Although the procedure is called an “embolization,” we are not closing the artery to the knee. The purpose of the procedure is to reverse the problematic increase in blood flow to the knee joint, which is causing inflammation. Essentially, our goal is to turn an “abnormal” artery back into a normal artery of the knee joint.
Angioplasty and stenting
Angioplasty uses an inflatable balloon catheter to open a narrowed vessel. Depending on the size of the plaque, the surgeon performing the procedure may decide to put a stent into the vessels to prevent it from closing up. With time, the blood flow in the affected area will be
restored. This is a surgical procedure that is performed in special laboratories or hospitals and requires anesthesia. You may have also had a stent placed. Please watch this video for more information:
https://www.youtube.com/watch?v=UOXQbF3K56g
Atherectomy
This includes a number of treatment methods that use special wire/catheter to remove plaques from the affected arteries. The plaques can be scraped, shaved, or cut by special catheter devices. The vascular surgeon will decide which method is more suitable depending on the location and morphology of the plaques. These are surgical procedures that grew in popularity
because of the available novel devices.
